From Fear to Freedom – Step by Step, Beat by Beat
Imagine your heart as a super‑powered pump. Its job? To send blood filled with oxygen and nutrients to every part of your body. But just like any pump, your heart has a strength level and that’s where ejection fraction comes in.
Listen here and read on for more ...
I remember the moment I first heard the term EF after my own heart event: it felt like reading a report card for my heart and wondering what that percentage meant for me. If you’re reading this, you might be asking the same question.
You may be feeling anxious, confused, or even overwhelmed by the medical language. Perhaps you’ve been told your ejection fraction is “low” or “reduced” and that can feel like the future is uncertain. The good news? You are not alone, and you don’t have to stay stuck in fear. You’re part of a journey toward finding your new normal.
A Way to Think about Ejection Fraction
It’s simply a measure of how much blood your heart is able to squeeze out with each beat. While the number is important, it doesn’t define you. With good care, mindset, and action, improvement is possible. Knowing the number gives you a starting place, a way to understand your heart’s current strength and how you might help it become stronger.
What is Ejection Fraction?
Ejection fraction (EF) is the percentage of blood that leaves your heart’s main pumping chamber, the left ventricle, each time it beats.
- Your heart fills with blood (diastole).
- It then squeezes (systole) to push that blood out to your body.
- The EF is the percentage of how much of the filled‑blood volume is actually pumped out.
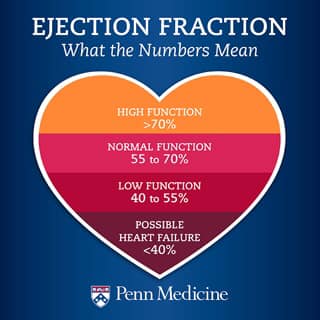
A “normal” EF is typically between 55% and 70%.
When EF is lower (for example below 40%), it can indicate that your heart is not pumping as strongly as it should.
It’s important to remember: EF is one piece of the puzzle, your heart is more than just a number.
Why Does Ejection Fraction Matter?
When your EF is low, your body might not be getting enough oxygen‑rich blood. That can mean you may feel:
- Tired or fatigued more easily
- Short of breath (especially with activity)
- Dizzy or light‑headed
These symptoms happen because your body’s needs aren’t being met.
Doctors use the EF number to:
- Understand how well your heart is working.
- Decide on treatments, lifestyle changes or monitoring that are appropriate.
- Check progress over time: Is your heart improving? Stabilising? Or is there more work to do?
How Is Ejection Fraction (EF) Measured?
Your cardiology team may use one or more of these tests:
- Echocardiogram (Echo): A painless ultrasound of your heart that shows how it pumps.
- MRI or CT scan: Provides detailed images of your heart’s structure and function.
- Nuclear Scan (MUGA or equivalent): Uses a small amount of radioactive tracer to assess pumping ability.
Your doctor will discuss the results with you; make sure you remember to ask for them in plain language if anything seems unclear.
Can You Improve Your EF?
Yes! There are ways to support and improve your Ejection Fraction
Medical Approaches
- Medications: Your doctor may recommend medications such as beta-blockers or ACE inhibitors. These can help your heart pump more efficiently, lower blood pressure, and reduce the overall strain on your heart.
- Heart Devices: In some cases, devices like a biventricular pacemaker or an implantable cardiac defibrillator (ICD) may be used to regulate heart rhythms and support heart function.
- Treating Root Causes: Addressing underlying conditions, such as high blood pressure, arrhythmias, or valve issues, can make a meaningful difference in your ejection fraction and overall heart health.
Lifestyle Strategies
- Regular, Safe Exercise: Engaging in doctor-approved physical activity, like a cardiac rehabilitation program, can strengthen your heart, boost energy, and enhance quality of life.
- Heart-Healthy Nutrition: A balanced diet low in sodium and excess fluids helps protect your heart and manage blood pressure.
- Weight Management: Maintaining a healthy weight reduces extra stress on your heart and supports overall cardiovascular health.
- Avoid Tobacco and Limit Alcohol: Quitting smoking and limiting or avoiding alcohol and recreational drugs gives your heart the best chance to recover.
- Stress Management: Techniques like meditation, Reiki, mindfulness, breathing exercises, or gentle movement can lower stress levels, which positively impacts heart function.

Actionable Tool: The “Heart‑Pump Boost” Activity
Here is a gentle, practical activity to help support your heart’s strength and mindset. Please remember, always work with your cardiologist or rehab team first.
Step‑by‑Step Instructions:
- Choose a quiet moment each day (even 5 minutes counts) when you can sit or lie comfortably.
- Close your eyes and take three slow, deep breaths, inhaling through your nose and exhaling through your mouth. Feel your heart area soften.
- For the next 2 minutes, with each inhale, imagine your heart expanding gently, and with each exhale, imagine it squeezing out that “used” blood and filling with fresh nourishment.
- After the 2 minutes, gently ask yourself: “How does my heart feel today?” Make a mental note or write one word (e.g., “steady”, “tired”, “better”, etc).
- Finish with a gentle affirmation: “My heart may have changed, but my capacity for joy hasn’t.”
Why this works (Positive Psychology / Mindset Principle):
- By focusing on your heart’s movement and giving it attention, you’re activating your mind‑body connection, which helps reduce stress and supports better circulation.
- The affirmation encourages a growth mindset: you’re acknowledging change, but reaffirming strength and possibility.
- Short, gentle practices like this help build confidence, especially when you might feel low energy or fatigued.
Benefits / Expected Outcomes:
- A calmer state of mind (less “racing thoughts” or anxiety about your heart).
- Increased awareness of your physical state (helping you recognise early signs of fatigue or imbalance).
- A sense of connection with your heart’s journey, a small but meaningful step toward emotional and physical empowerment.
Try this “Heart‑Pump Boost” activity once daily for a week. Notice how you feel beforehand and afterward. Maybe write down a single word or phrase that describes the shift.
Then ask yourself: “What’s one small thing I can do today to support my heart?” Perhaps it’s walking for 10 minutes, choosing a heart‑healthy snack, or simply resting when your body says so.
Remember: we’re moving step by step, beat by beat. Improvement may not be immediate or perfect and that’s completely fine. Small steps build into bigger ones.
Hope
Understanding your ejection fraction gives you real insight into your heart’s strength but it doesn’t define your future. With conscious care, mindset shifts, and steady steps, you can help your heart and your life move from fear to freedom. You’re not alone on this path. Your heart may have changed, but your capacity for joy, connection and purpose hasn’t. Let’s walk this journey together, finding our new normal and building a thriving life after heart disease.
From fear to freedom — one heartbeat at a time.